The COVID-19 pandemic has left many of us feeling impotent as we watch our friends on the front lines be forced to shift their attention to the most immediate needs, like finding enough PPE, tests, and beds. In these difficult times where it seems like the lowest-tech items are what stand in the way of providing care, it’s good to be reminded of the powerful role that healthcare technology has played in past pandemics. We can’t take for granted the massive lifesaving impact this technology is quietly making in the background. That’s heartening for those of us who work in healthcare tech. We find ourselves asking: how will the next generation of health technology like waveform AI be used to save lives and generate information during future outbreaks?
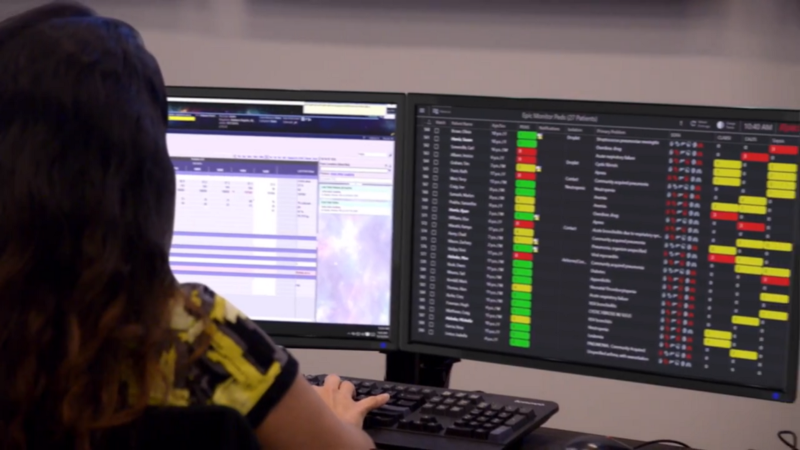
 Sentara was the first health system in the country to develop a tele-ICU, which they call eICU. Caregivers are the scarcest resource for coronavirus patients. Tele-ICU is helping them care for more patients. Providers can move from one patient to another with the click of a mouse rather than running down the hall and donning PPE. The mission-control-style room full of computer screens allows remote intensive care physicians and nurses to monitor 132 patients from a single workstation.
Now in its 20th year, the eICU program has helped lower mortality rates by 26.4% and shorten length-of-stay by 17%. It’s important to reduce length-of-stay even during normal times, when every day in the ICU is at best expensive and at worst both harmful and expensive. During a pandemic like COVID-19, when health systems have more critical patients than ICU beds, the stakes are even higher. Now, length of stay translates directly into lives — lives of people who would otherwise be turned away at the door or not receive the level of care they need.
Sentara was the first health system in the country to develop a tele-ICU, which they call eICU. Caregivers are the scarcest resource for coronavirus patients. Tele-ICU is helping them care for more patients. Providers can move from one patient to another with the click of a mouse rather than running down the hall and donning PPE. The mission-control-style room full of computer screens allows remote intensive care physicians and nurses to monitor 132 patients from a single workstation.
Now in its 20th year, the eICU program has helped lower mortality rates by 26.4% and shorten length-of-stay by 17%. It’s important to reduce length-of-stay even during normal times, when every day in the ICU is at best expensive and at worst both harmful and expensive. During a pandemic like COVID-19, when health systems have more critical patients than ICU beds, the stakes are even higher. Now, length of stay translates directly into lives — lives of people who would otherwise be turned away at the door or not receive the level of care they need.
 So how do we reduce length-of-stay in the ICU? After caregivers, the next-scarcest resource for hospitals in this pandemic is the supply of ventilators. Half of COVID-19 patients admitted to ICU require a ventilator. When these patients start getting better, they need to be weaned off of ventilator support. Weaning can start soon after intubation and takes from several hours to several days. During this process clinicians gradually step down the level of breathing help provided by the ventilator. As this happens the body’s mechanics gradually compensate to step up back to normal breathing function.
The interesting thing is that the lungs don’t do this on their own. Some of the most primal parts of our brain become active to facilitate the mechanical breathing compensation response. Researchers have shown that this activation occurs either at the same time as, or even precedes the optimal weaning time. This is where waveform AI comes in. AI will build on this research to more-accurately predict the optimal weaning time for a patient — using EEG waveforms to detect the right kind of activity in these parts of the brain. This has the triple benefit of reducing costs, bettering patient outcomes, and freeing the ICU bed sooner for the next patient who needs it.
The COVID-19 pandemic has many unknowns, and the lives of many caregivers and patients will be irreversibly impacted before it abates. Even as we feel powerless to stop it in the short term, we know from lessons of history that healthcare technology will improve outcomes for patients and healthcare workers alike.
So how do we reduce length-of-stay in the ICU? After caregivers, the next-scarcest resource for hospitals in this pandemic is the supply of ventilators. Half of COVID-19 patients admitted to ICU require a ventilator. When these patients start getting better, they need to be weaned off of ventilator support. Weaning can start soon after intubation and takes from several hours to several days. During this process clinicians gradually step down the level of breathing help provided by the ventilator. As this happens the body’s mechanics gradually compensate to step up back to normal breathing function.
The interesting thing is that the lungs don’t do this on their own. Some of the most primal parts of our brain become active to facilitate the mechanical breathing compensation response. Researchers have shown that this activation occurs either at the same time as, or even precedes the optimal weaning time. This is where waveform AI comes in. AI will build on this research to more-accurately predict the optimal weaning time for a patient — using EEG waveforms to detect the right kind of activity in these parts of the brain. This has the triple benefit of reducing costs, bettering patient outcomes, and freeing the ICU bed sooner for the next patient who needs it.
The COVID-19 pandemic has many unknowns, and the lives of many caregivers and patients will be irreversibly impacted before it abates. Even as we feel powerless to stop it in the short term, we know from lessons of history that healthcare technology will improve outcomes for patients and healthcare workers alike.
Categories: Blog, Technology
Share this post





